Despite tens of thousands of publication, accurate seizure detection in the EEG remains an unsolved challenge. Here are some of the reasons why this may be so.
The last decade has seen an enormous interest in the problem of seizure detection in the EEG. 35,000 journal articles have been published on the subject in all, of which almost 15,000 are within the last decade. Numerous competitions have been launched on Kaggle and elsewhere and yet it remains an unsolved challenge. Why so?
What Exactly is A Seizure?
When we think of a seizure the first thing that may come to mind is someone unconscious on the floor with their body stiff and shaking in a rhythmic motion. These are the most severe type of seizure – called tonic-clonic or grand mal seizures. However, what are called ‘seizures’ encompass a much broader range of symptoms such as sudden brief jerks or twitches of the arms and legs (myoclonic seizures), rhythmic jerking movements in the neck, face, arms (clonic seizures), sudden loss of muscle control (atonic seizures), sudden stiffening of the muscles (tonic seizures) and staring into space along with subtle movements such as eye blinking or lip smacking (absence or petit mal seizures). Other symptoms considered part of a seizure may include sudden confusion or anxiety, visual hallucinations such as seeing flashing lights, and the sensation of being ’out of body’. Essentially a ‘seizure’ is terminology for a very broad set of atypical movements as well as cognitive symptoms. Given such heterogeneity, it is not really one thing at all. Thus detecting ‘a seizure’ simply means detecting an abnormality that is brief in duration that generally involves some aspect of motor output, and maybe some other things too.
EEG during a Seizure
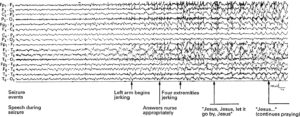
Given the broad range of symptoms that comprise a seizure, it is no surprise that to the visual eye the EEG can look quite different. Yet even within one general category of seizure there are differences. Below are examples of two different patients both with grand mal or tonic-clonic seizures along with an annotation of the events of the seizure from [1].
The first patient is a 44 year old male who experienced tonic-clonic seizures, at least from the perspective of limb movement, but remained conscious during the time and was able to speak, saying prayers through his seizure.
The second patient is a 16 year old male who reported dizziness and losing track of where his arm was in relation to the rest of his body.
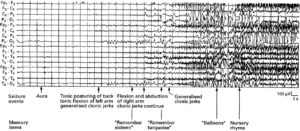
To the eye, the main difference that we can see here are an increase in the amplitude of the EEG across a wide range of signal. Sometimes like in patient 2 the EEG looks extremely different with some periods that are more rhythmic looking. On the other hand, this change is not as obvious in patient 1. There is a progressive difference to the eye in patient 2 but for anyone who has recorded lots of EEGs of people who are not experiencing seizure, it may be obvious that such changes in activity with increased amplitude do occur. Furthermore, both patients are conscious and retain some normal function so not every aspect of the brain function has gone awry.
‘Detecting’ a Seizure
The clinical diagnosis of a seizure in the EEG is typically determined by a trained clinician. What this means is that they have looked at hundreds of EEGs of folks who have come into their clinic with various seizure symptoms and developed some sort of idea of what ‘looks’ like a seizure. It is difficult to explain in any quantitative way, just a trained ‘sense’ of the EEG being ‘off’. Can we trust this kind of human intuition? Studies have shown that the ‘sense’ of different experts often don’t match. Which expert is right then? Nonetheless the field has pushed on. Clinicians eyeball the EEG and declare it normal or abnormal and mark out seizures.
With growing computing power and the advent of machine learning a whole field has now grown up to automate this detection of seizures. Yet they rely fundamentally on clinician annotations of seizures to train their models. What they are trying to do is find a way to describe what the clinician is intuiting. The false positive and false negative rates of the model therefore may therefore reflect less the failing of the model and more the failing of the clinician’s intuition to select something quantitatively consistent or because the seizures are too heterogeneous to be quantitatively consistent or both.
Psychogenic Nonepileptic Seizures
The biggest foil may come from what are known as psychogenic nonepileptic seizures or PNES. PNES are essentially seizures where the clinician cannot see anything ‘off’ in the EEG. The conclusion made is that these very same motor symptoms arise from some psychological factor but not the electrical activity of the brain. This contradicts the very foundation on which neuroscience is built which is that any type of motor behavior – normal or abnormal – arises as a consequence of electrical signals. If the abnormal motor behavior is not visible in the EEG as the roughly large amplitude signal that the clinician expects then what is that aspect of the seizure that is reflected in the EEG? It is not unconsciousness obviously since not all ‘seizures’ involve unconsciousness like the two examples above. It is not cognitive elements. Then what exactly?
The approach to seizures might be due for a complete rethink.
[1] William L Bell, Thaddeus S Walczak, Cheolsu Shin and Rodney A Radtke Painful generalised clonic and tonic-clonic seizures with retained consciousness Journal of Neurology Neurosurgery & Psychiatry January 1998