The Mental Health Million open data project is starting to highlight key features of our collective mental wellbeing. Here we summarize some early insights from the project including the effect of age, gender and Covid-19.
Over the past few months, the Mental Health Million (MHM) open data project has been making good progress in highlighting some of the key features of our collective mental wellbeing. The data we’ve collected so far (n=5493 to date) has predominantly been from respondents living in the United States (~50%), Canada and India (15% each), but across the database we have respondents from 101 different countries. This data is being collected using the Mental Health Quotient (MHQ) [1], a web-based all-in-one cross-disorder assessment tool which incorporates 10 mental health disorders and includes elements from RDoC, positive aspects of wellbeing and life context factors. Here we summarize some of the latest findings from the project.
Age
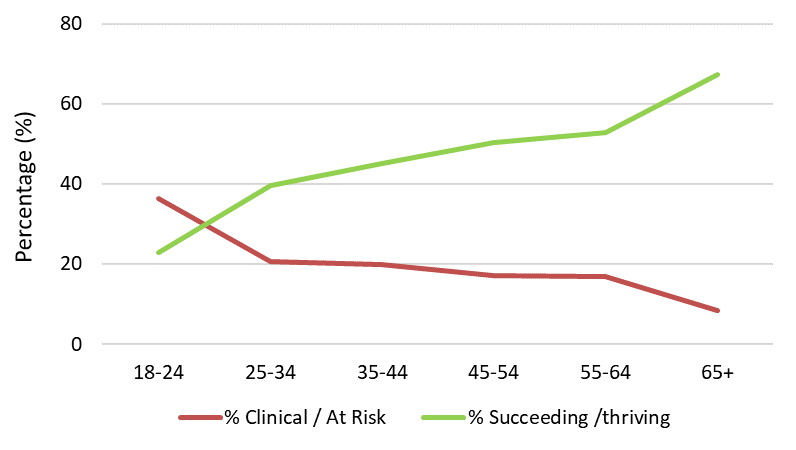
As suggested in other studies [2], the MHM project data is showing how the mental health of 18-24 year olds is considerably lower than for older age groups. In our latest round of analysis, 36% of 18-24 year olds have mental health scores at an “at risk” or “clinical” level while only 8.5% of those over the age of 65 have scores in this range. Conversely, only 23% of 18-24 year olds have mental health scores which are “succeeding” or “thriving” compared to 67% of those aged 65+. Although the profile of mental health challenges varies across respondents, some general trends are emerging, with sleep, self worth and anxiety being especially challenging to this younger age group. As our data collection progresses, we will be able to tease apart these differences to see how different mental health profiles might be related to different life contexts.
See related Post The Mental Health of Young Adults
Gender
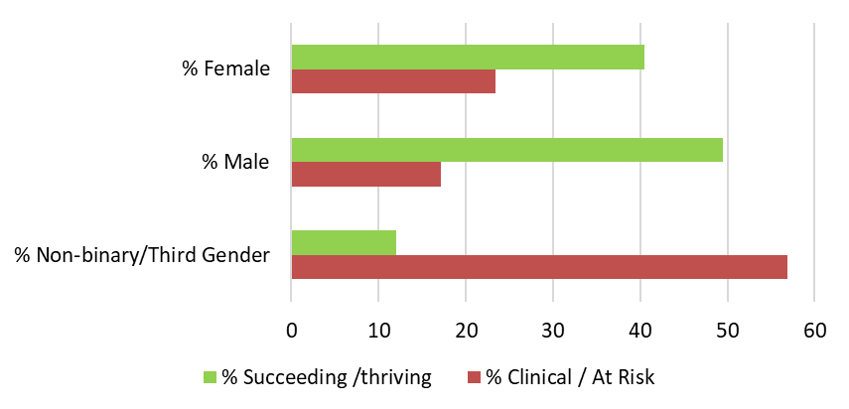
We also see that the mental health of female respondents is generally lower than male respondents, again in line with data from other sources [3-5]. The latest numbers indicate that 23% of female respondents and 17% of male respondents have mental health scores at an “at risk” or “clinical” level (Figure 2). For non-binary/third gender respondents the data collection numbers are still relatively low (n=58) but the data so far is striking with 57% of respondents in this group having “at risk” or “clinical” mental health scores.
Covid-19
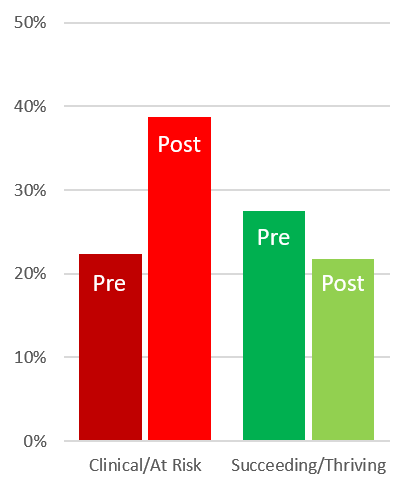
We did some initial data collection using the MHQ in July 2019 and are therefore able to compare current mental health trends against those seen before the Covid-19 pandemic. There have been several recent studies highlighting the negative impact of Covid on mental health (e.g. [6]) and this is a pattern we also see in the MHM data. Comparisons of pre-covid (before February 2020) and post-covid (after March 2020) responses show that 16% of the pre-covid cohort were in the “at risk” or “clinical” score range, while in the post-covid cohort, this number had increased to 24%. The increase was most striking in the 18-24 age group where the increase was from 22% (pre covid) to 39% (post covid) (Figure 2). The ongoing nature of the MHM project means we will be able to continue tracking evolving trends in mental health over the coming years.
Other Factors
Our data is also revealing differences based on other factors assessed in the MHQ. For example, this latest analysis indicates that mental health scores are higher for those who have a college education compared to those who left education after high school, and also highlights the association between sleep, exercise and face-to-face socializing with mental health and wellbeing. As we collect more data and explore factors in combination, we will be able to reveal a rich depth of insight into how these factors, and others, interact and relate to mental wellbeing. In addition, as translations of the MHQ become available (there are several in the pipeline) then we can start to map mental health and wellbeing across different geographies – one of the key objectives of the MHM project.
See related post The Mental Health Million Project.
Open Data Access
The Mental Health Million project is an open data project and researchers can contact us for access to the data. A data request form will also soon be available on the Mental Health Million Project page. As it is an ongoing project new data is added everyday at the rate of 200 to 500 responses per day.
Using the MHQ for Research
Understanding mental health at a population-level is only one use for the MHQ that we envisage. It’s been designed in a way so that the life context questions can be customized to different research needs beyond the MHM project. So as well as including standard questions on demographics and life experience, the questions in the assessment can also be tailored to specific research objectives, clinical profiles or population groups. It can therefore be used to help understand symptom profiles (it assesses 47 different mental symptoms and attributes), identify biomarkers or evaluate treatment outcomes. If you are an academic or not-for profit researcher looking for a new way to measure mental health and wellbeing, and are interested in using the MHQ in your research then please get in touch with us or take a look here for more information.
References:
[1] Newson, J., & Thiagarajan, T. (2020). Assessment of Population Well-Being With the Mental Health Quotient (MHQ): Development and Usability Study. JMIR Mental Health, 7(7), e17935. doi: 10.2196/17935
[2] Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068, NSDUH Series H-53). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2018. Retrieved from https://www.samhsa.gov/data/
[3] Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychological Bulletin. 2017;143(8):783–822. PMID: 28447828. doi:10.1037/bul0000102
[4] Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey I: Lifetime prevalence, chronicity and recurrence. Journal of Affective Disorders 1993;29(2-3):85-96. PMID:8300981. doi:10.1016/0165-0327(93)90026-g
[5] Van de Velde A, Bracke P, Levecque K. Gender differences in depression in 23 European countries. Cross-national variation in the gender gap in depression. Social Science & Medicine. 2010;71(2)305-313. PMID: 20483518. doi:10.1016/j.socscimed.2010.03.035.
[6] Pierce, M., Hope, H., Ford, T., Hatch, S., Hotopf, M., & John, A. et al. (2020). Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. The Lancet Psychiatry. doi: 10.1016/s2215-0366(20)30308-4
















