Transcranial magnetic stimulation can induce excitability and plasticity in the cortex with diagnostic and therapeutic applications in both neurological and mental health disorders.
Since the discovery that the brain communicates via electrical signaling scientists have tried ways of modifying and manipulating this signaling to understand brain function. Early efforts in humans at the turn of the 20th century, most notably by Wilder Penfield, involved the application of direct currents to the brain, initially applied directly to the brain surface during surgery. By stimulating the motor cortex for instance, one could evoke various movements of the limbs and other sensations.
See related post Stimulation, Sensation and Localization in the Cortex
It was only in 1980 that Merton and Morton [1] succeeded in electrically stimulating the motor cortex through the scalp in conscious humans. Using 2 electrodes connected to a high-capacity condenser (0.1 mF) charged up to 2000 V and placed on the motor cortex about 4 cm apart they were able to elicit a twitch in contralateral arm muscles with the application of current. Called Transcranial Electrical Stimulation or TES, it was an uncomfortable and painful procedure akin to receiving an electric shock. Furthermore, only some fraction of the current passed through the scalp and reached the cortex. Instead much of the current spread along the scalp evoking contraction of the scalp muscles and causing pain. It was therefore not a very viable approach.
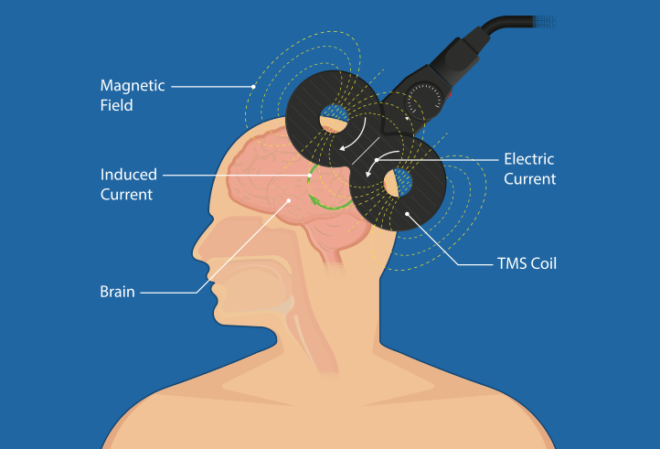
In 1985 an attempt was made to replace TES with TMS or Transcranial Magnetic Stimulation, essentially a non-invasive indirect method of inducing changes in excitability in the cortex via a wire coil generating a magnetic field of several Teslas that passes through the scalp [2]. The basic principle being that magnetic fields changing rapidly can induce circular electrical currents that flow in a plane perpendicular to the magnetic field. Unlike TES, it does not cause the same level of discomfort or induce pain and is relatively tolerable, though it does still feel strange. Much work has been done since then to demonstrate that TMS does indeed induce action potentials in neurons. Applied over the motor cortex it can elicit muscle twitching and movement that can be measured with EMG [3]. There are various kinds of TMS coil configurations including the circular coil, figure-of-eight coil, double-cone coil, air-cooled coil and, more recently, the Hesed coil,c-Core coil and circular crown coil.
TMS, Motor-neuron activation and Neurological Disease
TMS applied over the motor cortex induces descending volleys in the pyramidal tract projecting on to spinal motoneurons, also termed corticospinal tracts. The first motor neurons recruited by TMS of the motor cortex are also the same as those recruited during minimal voluntary contraction (from smallest to largest) which makes TMS a useful tool to measure changes in excitability in the corticospinal excitability in neurodegenerative disease such as ALS which typically starts with motor neuron degeneration [4]. Practically, the excitability of corticospinal pathways is estimated as the minimum TMS intensity required to evoke a muscle response or MEP of at least 50 mV in about 50% of 5 to 10 consecutive trials using a two pulse TMS protocol. Other protocols such as high frequency repetitive TMS (rTMS) protocols can induce excitability and help in enabling rehabilitation of Stroke and retard progression of Multiple Sclerosis. It has also been used to treat pain by applying it to the motor cortex contralateral to the region of pain.
TMS, Plasticity and Mental Health Disorders
In general, certain protocols of electrical stimulation of neuronal tissue can induce plasticity. By extension, some protocols of TMS should be able to create changes in the neuronal network as well. Using this as a principle, TMS has been used in the treatment of major depressive disorder (MDD) with protocols such as repetitive TMS (rTMS) applied to the prefrontal cortex at a frequency of 5-10 Hz with reasonable efficacy [5]. Other protocols such as intermittent theta burst stimulation (iTBS) is also sometimes used in MDD with success. Going forward the applications of TMS are likely to extend beyond MDD to other mental health disorders. A recent study in cats using a voltage-sensitive dye has shown that using a high-frequency (10 Hz) TMS protocol, they were able to transiently destabilize the cats visual cortical maps and sensitize the cortex to a bias in input (here a prolonged single visual orientation) in order to relearn connectivity patterns [6]. This suggests that in the future one could potentially use TMS to disrupt certain learned patterns or responses and prime towards others.
References
[1] Merton PA, Morton HB. Stimulation of the cerebral cortex in the intact human subject. Nature 1980; 285:27.
[2] Barker AT et al, Non invasive stimulation of the motor cortex. Lancet 1985;2:1106–7.
[3] Hess CW et al, Responses in small hand muscles from magnetic stimulation of the human brain. J Physiol 1987; 388:397–419.
[4] Henneman E, Mendell LM. Functional organization of the motoneuron pool and its inputs. In: Brooks VB, editor. Handbook of Physiology Section I The Nervous System Motor Control Part 1, vol. II. MD: American Physiological Society Bethesda; 1981.
[5] Shawn M. McClintock et al, Consensus Recommendations for the Clinical Application of Repetitive Transcranial Magnetic Stimulation (rTMS) in the Treatment of Depression, J Clin Psychiatry. 2018 79(1)
[6] Vladislav Kozyrev et al, TMS-induced neuronal plasticity enables targeted remodeling of visual cortical maps PNAS June 19, 2018 115 (25) 6476-6481