How does mental wellbeing differ across genders? Data from the mental health million project describes a diminishing gender gap with age and specific dimensions of difference.
Estimates from large-scale epidemiological studies such as the Global Burden of Disease study [1] and National Comorbidity Survey (NCS) [2] often highlight that females report a higher prevalence of mental health disorders compared to males, especially when it comes to mood disorders such as depression and anxiety. A recent meta-analysis of national surveys, looking specifically at depression found a gender difference (with higher prevalence in women) that emerged during adolescence, declined during adulthood and then remained stable [3]. However, the picture isn’t as straightforward for other disorders, and there are also additional factors which play a role in the difference in prevalence between men and women. For example, developmental disorders such as autism spectrum disorder (ASD) are more commonly diagnosed in males compared to females [4], while gender differences have been reported for trajectories of disorders such as schizophrenia [5]. Furthermore, while suicidal ideation is often reported to be higher in women, suicidal intent and mortality are higher in men [6,7] with other studies suggesting that men are often more reticent to speak out about their mental health challenges [8]. The Mental Health Million Project takes a different look at gender differences, not just in relation to individual disorders, but across the spectrum of mental wellbeing from clinical to thriving.
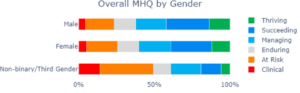
Those who identify as non-binary/third gender report the lowest mental wellbeing.
Across all 50k+ adults who have completed the MHQ so far, there is a small difference in mental wellbeing between males and females, a gender gap that is relatively small at just 4 points. In contrast those who identify as non-binary/third gender report the lowest mental wellbeing across the board, with a shocking magnitude of difference of 40+ points. A higher prevalence of mental health disorders in non-binary/third gender has been reported previously [9,10]. What is striking in this data however is the magnitude of difference. Those who are non-binary have a are more than three times as likely to have a clinical disorders and twice as likely to be at risk for a clinical disorder.
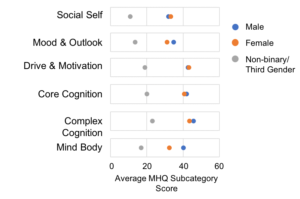
The gender gap across functional domains
Also of interest is that the gap between males and females is not uniform across functional domains. There was no significant difference along the dimensions of Social Self, Drive & Motivation and Core and Complex Cognition. On the other hand women had lower scores on average in the domains of Mood & Outlook and Mind Body Connection. In contrast, those who were Non-binary had poorer scores across all functional domains.
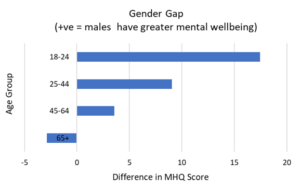
The gap between males and females decreases with age.
One interesting aspect of the male-female gender gap is that it changes profoundly with age. The gap is greatest for those aged 18-24 with females reporting lower mental wellbeing compared to males by ~17 MHQ points. This gap decreases to 9 points for those aged 25-44 and to 4 points for those aged 45-64. For those aged 65+ the gender gap reverses, with males reporting lower mental wellbeing, though the difference is fairly small (3 MHQ points).
See related post An Early View of Results from the Mental Health Million Project
What drives the gender gap?
The reasons behind these differences across age and dimension are still not fully clear although a range of interacting social, environmental and biological factors are likely to play a role. These may also vary across population subgroups which could provide insights into whether the key drivers are biological or socio-cultural. It is one of the aims of the Mental Health Million project to tease apart some of these factors to improve our understanding of the drivers of mental wellbeing across the globe.
References
[1] https://www.thelancet.com/gbd
[2] https://www.hcp.med.harvard.edu/ncs/
[3] Salk, R. H., Hyde, J. S., & Abramson, L. Y. (2017). Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychological bulletin, 143(8), 783–822.
[4]Loomes R, Hull L, Mandy WPL. What Is the Male-to-Female Ratio in Autism Spectrum Disorder? A Systematic Review and Meta-Analysis. J Am Acad Child Adolesc Psychiatry. 2017 Jun;56(6):466-474.
[5] Sommer, I.E., Tiihonen, J., van Mourik, A. et al. The clinical course of schizophrenia in women and men—a nation-wide cohort study. npj Schizophr 6, 12 (2020).
[6] Freeman, A., Mergl, R., Kohls, E. et al. A cross-national study on gender differences in suicide intent. BMC Psychiatry 17, 234 (2017).
[7] Naghavi M. Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016 BMJ 2019; 364 :l94
[8] Galdas PM, Cheater F, Marshall P. Men and health help-seeking behaviour: literature review. J Adv Nurs. 2005 Mar;49(6):616-23.
[9] Cochran SD, Mays VM, Sullivan JG. Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. J Consult Clin Psychol. 2003 Feb;71(1):53-61. d
[10] Russell, S. T., & Fish, J. N. (2016). Mental Health in Lesbian, Gay, Bisexual, and Transgender (LGBT) Youth. Annual review of clinical psychology, 12, 465–487.