The DSM is a theoretical framework for grouping of symptoms into disorder classifications. How well does it match the real-life diversity of symptom presentation?
Across clinical and research domains, mental health assessment is typically carried out using interviews and questionnaires whose content is based on classification systems (e.g. DSM-5 or ICD-11) where patterns of symptom criteria have been grouped together and designated as specific mental health disorders. However, although this classification approach offers clinical utility, it is at odds with the heterogeneity of symptom presentation and the realization that comorbidity is the norm, rather than the exception [1,2]. So the question is, how true actually are these disorder classifications to real-life symptom profiles?
Mapping MHQ symptom profiles to the DSM
See related post: 3 Challenges in Mental Health Assessment
To examine this, we turned to data collected using the MHQ, our online mental health assessment tool that, for each individual, produces a comprehensive symptom profile containing 47 items that span the breadth of mental health and wellbeing. It also utilizes a nonlinear scoring algorithm to determine where that individual falls on the spectrum from clinical to thriving. As the MHQ has been designed based on an analysis of 126 existing DSM-based mental health questionnaires and interviews spanning 10 disorders [3], the symptoms that the MHQ asks about can be readily mapped to DSM criteria [4]. Although this mapping is only done on the symptom content, rather than on the duration of the symptoms, it nonetheless allows us to get an indication of how a person’s symptom profile, derived from the MHQ, aligns with the different criteria associated with 10 of the most common DSM-based disorders. When this is done across a large group of respondents, it can tell us about the general goodness-of-fit between DSM disorder criteria and real-life symptom profiles.
We therefore examined a large set of symptom profiles taken from ~10,000 MHQ respondents and mapped their profiles against DSM criteria. This mapping was done, first, by aligning items from the MHQ against symptoms included in the DSM criteria and developing a series of rules which reflect those criteria. This was done for 10 different disorders – depression, anxiety, bipolar disorder, ADHD, addiction, autism spectrum disorder, obsessive-compulsive disorder, post-traumatic stress disorder, schizophrenia and eating disorder. These rules were then applied to the individual symptom profiles derived from the MHQ, using a thresholding approach where only symptoms that were having a severe impact on a person’s ability to function effectively in life were considered.
Vast Comorbidities: Many symptoms profiles match to multiple disorders
What we found was that there was a huge diversity of disorders associated with symptom profiles. For 81% of MHQ respondents who were within the “clinical” category, their profile of severe symptoms aligned with more than 1 disorder (see figure 1a). For those who were in the “at risk” category and whose profile of severe symptoms aligned with at least 1 disorder, the results showed that 45% of these profiles aligned with 2 or more disorders (see figure 1b). This suggests that although there is alignment between DSM criteria and symptom profiles, the vast overlap of these profiles across multiple disorder criteria, suggests that single disorder labels rarely reflect the true symptom experience of the individual. Note that there is vast overlap in symptom criteria across DSM disorders [3].
Falling Between the Cracks: Many with severe symptoms have no DSM- disorder
We then turned to look at those respondents who were also in this clinical or at-risk group but whose profile of severe symptoms did not align with any DSM disorder criteria. This applied to 6% of those in the clinical group and 60% of those in the at-risk group. We found that these respondents nonetheless experienced a high number of severe symptoms with 100% of this clinical subgroup and 51% of this at-risk subgroup reporting 5 or more severe symptoms (see figure 2). Many of these symptoms fall within the criteria of the broader DSM but simply do not fit any particular disorder grouping. Although we only included the criteria for 10 disorders, and it might be the case that their symptoms align with criteria for other disorders that we did not look at here, it also raises the question as to whether these are people with atypical symptom profiles who risk “falling through the gaps” of the current classification system.
Implications
The mismatch between DSM disorder classifications and the symptom profiles of individuals apply have implications not only to the diagnosis of mental health disorders, but also in terms of treatment decisions. Although clinicians have a wealth of knowledge and work-arounds to select treatments regardless of DSM-disorder labels, this results in a lack of standardization across the field and prevents clear joined-up thinking as to which treatments would be best for which patients. The MHQ offers a standardized assessment of mental health that is based on symptom profiles, helping to form a bridge between existing diagnostic systems and newer transdiagnostic frameworks, and which we believe will ultimately lead to more precise treatment selection that is closer to the needs of the individuals.
You can hear more about these issues surrounding diagnosis and treatment of mental health disorders at our upcoming virtual symposium on The Future of Mental Health: Measurement, Treatments and Therapies.
References:
[1] Maj M. ‘Psychiatric comorbidity’: an artefact of current diagnostic systems? Br J Psychiatry (2005) 186(3):182–4. doi: 10.1192/bjp.186.3.182
[2] Plana-Ripoll O, Pedersen CB, Holtz Y, Benros ME, Dalsgaard S, de Jonge P, et al. Exploring comorbidity within mental disorders among a danish national population. JAMA Psychiatry (2019) 76(3):259–70. doi: 10.1001/jamapsychiatry.2018.3658
[3] Newson, J., Hunter, D., & Thiagarajan, T. (2020). The Heterogeneity of Mental Health Assessment. Frontiers In Psychiatry, 11. doi: 10.3389/fpsyt.2020.00076
[4] Newson, J., & Thiagarajan, T. (2020). Assessment of Population Well-Being With the Mental Health Quotient (MHQ): Development and Usability Study. JMIR Mental Health, 7(7), e17935. doi: 10.2196/17935


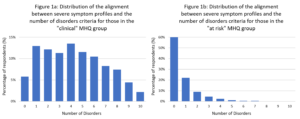
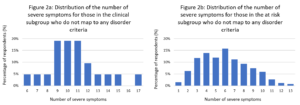
Figure 2A and 2B repeated twice. Figure 1A and 1B missing
Thanks for pointing that out. It is now fixed.