Two people with depression can have vastly different symptom profiles. How can they be grouped together in terms of clinical treatment or recruitment into trials? Understanding empirical symptom profiles can help reduce trial-and-error.
It’s well established that the use of disorder-based classification systems is at odds with an understanding of the true range and diversity of symptom profiles present across clinical populations as the objective is to narrow down to a single label rather than embrace the range of symptomatic experience.
See related articles How true are DSM disorder classifications to real-life symptom profiles? And The Vast Comorbidities of Mental Health Disorders
However, within clinical populations, it’s likely that the nuances of someone’s profile of symptoms hold important insights that can help guide clinical decision-making and so there is a real need to better understand the range and diversity of clinical symptom profiles to inform the narrative around mental health.
Two people with depression
Below are the symptom profiles of two people with the same number of symptoms who meet the criteria for depression.
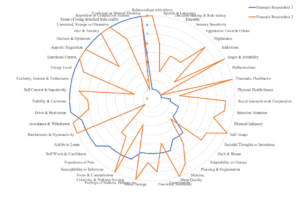 Figure 1: Ratings of Symptom Severity on a Life Impact Scale. Very severe symptoms (8 or above) are considered clinically relevant for diagnosis.
Figure 1: Ratings of Symptom Severity on a Life Impact Scale. Very severe symptoms (8 or above) are considered clinically relevant for diagnosis.
How does one interpret this? Do they simply get treated the same?
From the perspective of the DSM, it has long been realized that ‘comorbidity’ or the presence of positive diagnosis for multiple DSM-classified disorders is the norm. Do we see these two people as both having depression but also additional disorders that are different? Or simply people having two very different symptom profiles that may thus reflect distinct underlying etiologies.
Is it more valuable to say one person has depression comorbid with anxiety and ADHD and another has depression comorbid with eating disorder? If expressed in terms of the percentage of symptoms of each DSM-based disorder classification, each individual may have anywhere from 15-40% of symptoms of each disorder. Or is it more informative to understand how constellations of symptoms present across the population?
Empirical Mapping of Symptoms
Large scale multidimensional population data allows an ability to explore the empirical presentation of symptoms in a different way. As part of the Mental Health Million project we are currently using a large open dataset of ~112,000 individuals across the general population who completed the Mental Health Quotient (MHQ), to better understand the diversity of their symptom profiles. To do so we’re mapping the different items from the MHQ (thresholded for clinical significance) to the diagnostic criteria of 10 different mental health disorders taken from the DSM-5. As the MHQ was originally derived from assessments from these disorders [1], we can then use the data to identify MHQ symptom profiles that map to each disorder. Although this mapping does not categorically state that the individual would be diagnosed with that disorder in the context of a clinical interview, it does broadly tell us that their pattern of symptoms aligns with the diagnostic criteria for that disorder.
By then looking at the range and diversity of symptom profiles that map to any one disorder, we’ll be able to see the true heterogeneity of patient experiences across this population that are associated with a particular disorder label. Beyond this we can then look at how many symptom profiles map to more than one disorder, giving us a feel for the extent to which comorbidities are present within the population.
The consequence of ignoring empirical symptom profiles
The outcome of this project will have considerable implications for how we consider mental health challenges from epidemiology to clinical diagnosis and research.
Currently, given all the heterogeneity of symptoms, practical implementation of DSM-5 criteria in a clinical setting is fraught with challenges that clinicians must circumvent when making a diagnosis. This means that a relatively low proportion of clinicians (39%) report often or always referring to written DSM criteria during an initial evaluation [2] and approximately a third often or always use not otherwise specified (NOS) categories, primarily due to the patient not meeting criteria for a specific category. What this means is that the ‘diagnosis’ you get depends more on the doctor than any standardized criteria – really a trial-and-error approach.
Clinical research that depends on this criteria is also not likely to fix this challenge. For instance, when simple screens such as the PHQ-9 are used to recruit people into a depression trial, both individuals above could technically form part of the depressed group. Should we expect that both people above would react the same way to a treatment? When the results are noisy and not very strong, should we be surprised? So also it hinders the identification of biomarkers and may be a key reason behind the very ambiguous and general results of EEG profiles across disorder groups (see related post EEG Frequency Bands across Mental Health Disorders).
Moving towards empirical symptom profiles
There is therefore a real need for a system of symptom profiling that is closer to the needs of the patient and the clinician. Within the research domain, where researchers have already started to look at symptom networks [3], symptom profiling can also help to segment clinical groups by profiles rather than diagnostic labels, allowing for trials of treatments on more homogenous groups and aiding the search for underlying etiologies and more personalized treatments. At the very least, it can reduce trial-and-error.
We will report on the outcome of this project in the coming months – stay tuned!
References:
[1] Newson JJ, Thiagarajan TC Assessment of Population Well-Being With the Mental Health Quotient (MHQ): Development and Usability Study JMIR Ment Health 2020;7(7):e17935
[2] First MB, Erlich MD, Adler DA, Leong S, Dixon LB, Oslin DW, Goldman B, Koh S, Levine B, Berlant JL, Siris SG. How the DSM Is Used in Clinical Practice. J Nerv Ment Dis. 2019 Mar;207(3):157-161.
[3] Borsboom D. A network theory of mental disorders. World Psychiatry. 2017 Feb;16(1):5-13. doi: 10.1002/wps.20375.