Epilepsy is a widespread disorder but identifying and predicting seizure onset still eludes us. Continuous tracking with mobile EEG may soon begin delivering some answers.
Epilepsy is one of the oldest-known and most widespread neurological disorders in the world. It is a term used to describe the repeated occurrence of “seizures”. Outwardly the most obvious and frightening seizures are Grand Mal Seizures where the person loses consciousness and convulses with violent muscle contractions. However seizures are varied and sometimes hard to pin down. They can be as small as a repetitive muscle twitching to a period where the person simply stares. There are wide variations in terms of how each individual seizure can manifest itself – something that depends on the particular region of the brain involved and the extent and spread of the electrical discharge. Indeed it has been said that any activity that the brain can do can become a seizure – i.e. a period where a region of the brain gets locked into a something of a repetitive loop or abnormal behavior. Common to all seizures however, is their unpredictability. It is this that makes epilepsy so life-threatening and debilitating through accidents and injuries, especially when seizures occur multiple times a day, as they do in some more severe cases.
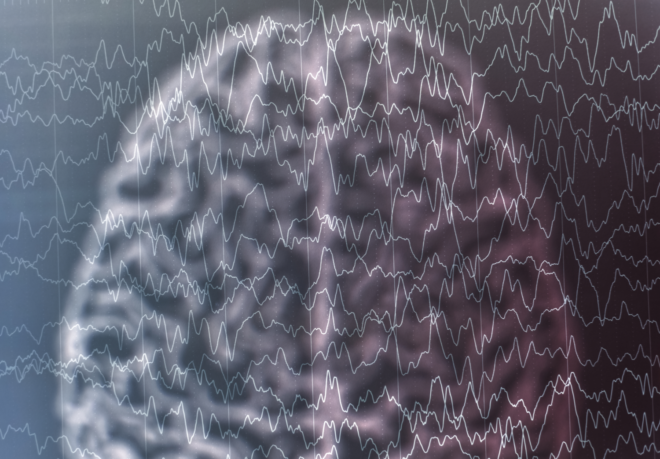
Using EEG to measure epilepsy.
The epileptic brain’s regional hyperexcitability can, in most instances, be seen within an continuous EEG recording by way of regionally specific spikes or sharp waves (as well as array of other possible neural features). Analyzing an ongoing EEG is therefore typically one of the most common diagnostic methods for the detection of epilepsy.

(From: http://www.sciencedirect.com/science/article/pii/S1525505009000924)
There are typically two phases of neural features associated with an epileptic seizure which researchers can try and identify within an EEG waveform – those which are “pre-ictal” (immediately before the seizure) and those which are “ictal” (during the seizure). In general scientists believe that during the pre-ictal stage, there is a reduction in the connectivity between neurons in the brain region where the seizure it about to occur – the epileptogenic zone. This results in the neurons becoming isolated from the wider neural circuitry which ultimately results in them momentarily becoming separated from the inhibitory control which usually keeps them in check. This then leads to sudden neural excitation, or discharge, which results in an epileptic seizure.
While there is some agreement on these general theories, there is much argument over the identification of a seizure in the EEG. Significantly there is an intense search to identify and predict their onset with sufficient time so that patients can either prevent it by taking medication or find a safe place to ride it out.
[See related post What does the EEG signal measure?]
The dynamical features of an epileptic brain.
Because seizures occur abruptly and unpredictably, they are difficult to catch on EEG during a routine EEG in a clinic unless the patient happens to have a seizure during the session. Instead algorithms attempt to identify markers that may signal a propensity for seizure – picking out “interictal” neural abnormalities which occur between seizures. Although there are various behaviors which can increase the likelihood of observing these features (e.g. sleep deprivation), isolating them from within a “noisy” EEG still remains a real challenge to epilepsy researchers, given the high degree of interictal feature variability that can be observed between individuals.
Researchers have therefore started to seek out methods which allow more real-time longitudinal recordings of the epileptic brain outside the clinic environment, as well as developing more automatic methods for trying to the detect these features within the EEG. These advances aim to help minimize the risk of misdiagnosis and confirm that the seizure is not due to some other underlying disorder or disrupted health state. They could also be useful for measuring the effectiveness of any pharmacological intervention at an in-vivo biological level.
Tracking seizures on the go
Jessica Askamp and Michel van Putten from the University of Twente in the Netherlands recently performed an evaluation of a mobile EEG device – the Mobita – in the home to provide longitudinal measurements on a range of patients who had, or were suspected to have, epilepsy.
[See related post Taking Neurotechnology out of the Lab]
To complement this they also questioned clinicians and patients about the use of mobile-EEG as part of the patient monitoring regime. The revealed that there is great potential for using mobile EEG devices in epilepsy research and clinical monitoring, especially where the clinical diagnosis or interictal features are less clearcut. However, the challenges of analyzing the EEG to identify the many different epileptic features – already difficult within a clinical settings – are further complicated within a mobile environment where movement artifacts are greater and where automated algorithms are less readily available. The field is ripe for technological innovation to support this in the future.
The diagnosis of epilepsy is only the start of a long road of trying to reduce and manage the repeated neural excitabilities which can have such a disruptive and potentially fatal impact on people’s lives. Pharmacological treatments can help to reduce the frequency of seizures, meaning that many people can continue to live their normal lives, but they do not work in all cases. Taking EEG out of the lab, and developing automatic algorithms which don’t just accurately detect when a seizure has occurred, but which actually predict when one might happen before it even does so, is a challenge that is high on the wish list of those trying to successfully manage their epilepsy on a daily basis.