The microbiome is vast and we are only now beginning to understand the breadth of influence they have on the brain.
The human body has as many bacteria as human cells, most of which are intestinal residents. The number of resident bacteria species are enormous and collectively have an astonishing 232 million genes among them, compared to the estimated ~20,000 genes in the human genome. Altogether, they are not simply mooching parasites on the human body but play an active role in expanding the metabolic potential of humans. They sense a vast array of chemical signals and signal responses that have impact throughout the human body. What do we know about their influence on the brain and what are the big challenges?
See related post The Rat Size Brain in Your Gut
Key Bacterial Modulators of Nervous System Function
Thus far a handful of key brain related molecules that are influenced by specific gut bacteria have been identified and studied. These are Oxytocin, BDNF, GABA, 4-EPS and SCFA – which represent a highly varied set of molecules.
Oxytocin is a hormone produced in the hypothalamus that has been associated with maternal-new-born bonding and social behavior. A bacteria called Lactobacillus Reuteri seems to act by increasing oxytocin levels in the plasma to recover deficits in social behavior caused by maternal high fat diets – well, at least in mice [2]. This suggests a potential role in Autism related symptoms.
BDNF (Brain-Derived Neurotrophic Factor) is a protein encoded by the BDNF gene. It is a neurotrophic factor (i.e. it influences nerve growth) and is therefore implicated in learning and memory. This is regulated by a bacteria called Bifidobacterium longum NCC3001. Some evidence also suggests a link to depression and anxiety like behavior in rats, and maybe humans.
GABA is a naturally occurring amino acid that acts as a neurotransmitter, particularly in inhibitory synapses. Its therefore important in maintaining the balance of excitation and inhibition, crucial for effective transmission of neural signals. A gut bacteria called Lactobacillus Rhamnosus actually produces GABA and thereby regulates GABA-A and GABA-B receptors.
4-EPS (4-ethyl phenyl sulfate) is a metabolite of certain gut bacteria that is also a uremic toxin (a metabolite that is filtered and excreted by the kidneys and in high levels can be toxic). On the other hand, it is known to be reduced at least by one bacteria, Bacteroides fragilis, which seems to have anxiety reducing effects in mice.
Finally, there are Short Chain Fatty Acids (SCFAs) which regulate genes needed for the maturation and growth of microglia. Glia of course, which have all kinds of significant roles in the brain. These SCFAs are produced by various gut bacteria.
See related posts Astrocytes in Charge and Astrocytes Mediate Brain Lymphatic Function
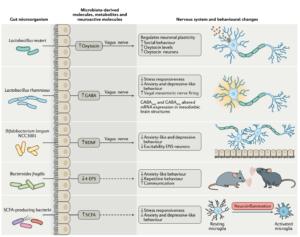
Figure 1: From [1]
Everything is suggestive, nothing is certain
The challenge however is that everything is suggestive, and nothing is certain.
First, as you can see, the type of molecules that are influenced by bacteria are varied – from synthesized hormones and genetically encoded proteins to amino acids and toxic metabolites. This suggests a very vast landscape of possibility where these represent only the very tip of the iceberg.
Second, a single bacteria out of tens of thousands in the gut most likely does not tell the whole story. With so many bacteria, encoding millions of genes and producing so many metabolites, who is to know if the ones that have been identified are the most important. And then there are interactions between them that we have yet to understand.
Third, even with these well studied bacteria and molecules above, much of the research relating to disease and mechanism has been done in rodents and how this translates to the human context is unknown. Finally, in the few human studies the results may show significant differences between groups but these are neither large nor definitive differences at an individual level. Studies of BDNF in depression for instance are not terribly conclusive – BDNF seems to increase after some therapies but not others and in some studies but not others [3]. In a randomized control study probiotic supplements of Bifidobacterium longum NCC3001 given to people with irritable bowel syndrome reduced depression scores in 14 out of 22 people by 2 points or more on the HAM-D scale. These are neither large nor conclusive numbers.
From single molecules to big data approaches
Companies that offer microbiome testing now characterize over 20,000 bacteria in the gut. Many studies are now going after changes in the comprehensive profiles with various diseases. However, with such a complex system, it will take large scale studies and personalized approaches, particularly with respect to the brain. Understanding when it comes to the brain will come eventually – but it is not here yet. Beyond the challenge of the complexity of the microbiome, this understanding is also hindered by the poor definitions and classifications of disorders to begin with. A lot of work lies ahead.
See related posts The Challenges of Mental Health Diagnosis and What Are Mental Disorders?
References
[1] Morais, L. et al., The gut microbiota–brain axis in behaviour and brain disorders, Nature Reviews Microbiology, 2021
[2] Sgritta, M. et al, Mechanisms underlying microbial-mediated changes in social behavior in mouse models of Autism Spectrum Disorder, Neuron 2019
[3] Arosio B. et al., Blood Brain-Derived Neurotrophic Factor (BDNF) and Major Depression: Do We Have a Translational Perspective? Front Behav Neurosci. 2021 Feb 12.
[4] Pinto- Sanchez, M. I. et al. Probiotic Bifidobacterium longum NCC3001 reduces depression scores and alters brain activity: a pilot study in patients with irritable bowel syndrome. Gastroenterology, 2017.

















Having mice be the subject of the majority of such R&D is unsettling as mice have tails that feed key sensory information to their brains differently than a human subject. Such a key difference in the anatomical structure of these two species has to impact research findings.
Additionally, mice scurry on all fours, have different culinary taste buds and smell-linked cellular memory. This definitely does not allow research to compare apples with apples. Sometimes I wonder if such a propensity to apply mouse-related research findings to bi-pedal humanality just may be inadvertently creating a type of evolutionary ‘convergence’ that is altering the very nature of humanity. Would love to learn more about this.
Hi, pretty cool in the context of the diversity of the Indian context.